Introduction to Diabetes: The Unseen Iceberg
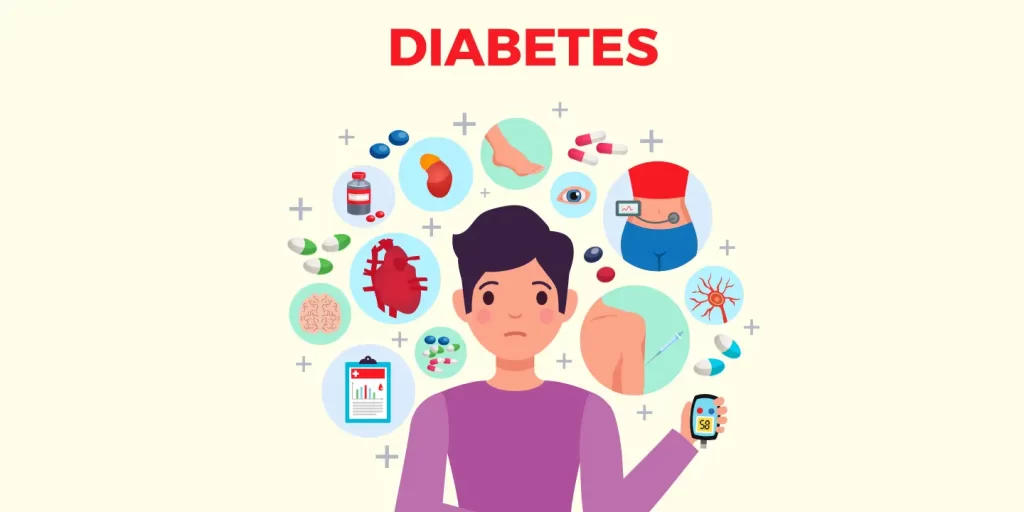
Imagine an iceberg. The tip represents the visible symptoms of diabetes – frequent thirst, hunger, and urination. But what about the bulk hidden beneath the surface? That’s the vast, often unseen, impact of diabetes on the body, affecting everything from your heart and kidneys to your eyes and nerves.
Table of Contents
Diabetes is a chronic metabolic condition where your body either can’t produce enough insulin (Type 1 Diabetes) or can’t use insulin effectively (Type 2 Diabetes). Insulin, a hormone produced by the pancreas, plays a key role in converting glucose from the food we eat into energy. Without sufficient insulin activity, sugar builds up in the bloodstream, leading to high blood sugar or hyperglycemia – the cornerstone of diabetes.

Step-by-step on How to Avoid Diabetes: The Art of Dodging the Bullet
- Eat Healthily: The first step is embracing a balanced diet. Imagine your body as a luxury car. Would you fill it with cheap fuel? Of course not! Similarly, fill your body with nutrient-rich foods like fruits, vegetables, whole grains, and lean proteins.
- Stay Active: Just like a river that flows is cleaner than stagnant water, an active body manages insulin better. Regular physical activity, be it brisk walking, swimming or yoga, can significantly lower your risk.
- Maintain a Healthy Weight: Think of your body as a ship. Excess weight is like carrying too much cargo, making it harder for the ship to navigate. Shedding even a few pounds can make a difference.
- Quit Smoking: Smoking can be seen as the pirates of the body’s ship, damaging the body from inside, increasing the risk of diabetes.
- Limit Alcohol: Just as you wouldn’t want to flood your engine with oil, don’t drown your body in alcohol. Excessive drinking can lead to weight gain and increase your diabetes risk.
Step-by-step on How to Manage Diabetes: Navigating the Storm
- Monitor Your Blood Sugar: Regular checks act like a GPS, helping you understand where you’re at and where you need to go with your diabetes management.
- Healthy Eating: Just as you wouldn’t put diesel into a petrol car, you need the right fuel – a diet rich in fruits, vegetables, lean proteins, and less processed food as per M. Regina Castro, M.D.
- Regular Exercise: Think of exercise as the engine tuner, it helps your body use insulin more efficiently, lowering your blood sugar.
- Take Your Medication: These are your body’s pit crew, helping to keep everything running smoothly. Always take prescribed medications as directed by your healthcare provider.
- Manage Stress: Stress can rev up your engine, raising your blood sugar. Practice stress management techniques like meditation and deep breathing.
List of Over-the-counter Medications for Diabetes
Some OTC medications for diabetes include:
- Metformin
- Glipizide
- Glyburide
- Insulin Aspart (NovoLog)
- Insulin Lispro (Humalog)
Always consult your doctor before starting or stopping any medication.
Why is it Important to Manage Diabetes?
Imagine a car left untuned and unchecked; it gradually loses its efficiency, right? Similarly, uncontrolled diabetes can lead to severe complications over time, such as heart disease, kidney damage, nerve damage, eye damage, and even stroke. By managing your diabetes, you’re not just taming the symptoms; you’re keeping the whole body’s engine running smoothly and efficiently.
What are Misconceptions about Diabetes?
- Myth: Diabetes is not a serious disease: Diabetes is like a wolf in sheep’s clothing. It might seem harmless initially, but if left uncontrolled, it can lead to serious health complications.
- Myth: Eating too much sugar causes diabetes: While a diet high in sugar can lead to weight gain and increase the risk of Type 2 diabetes, it’s not the sole cause. Factors like genetics and lifestyle play significant roles.
- Myth: People with diabetes can’t eat sweets or chocolate: Imagine your diet as a music playlist; it’s all about balance and variety. People with diabetes can enjoy sweets or chocolate in moderation, as part of a balanced diet.

FAQ’s with Answers on Diabetes
- Can diabetes be cured? As of my knowledge cutoff in September 2021, there’s no known cure for diabetes. However, it can be effectively managed.
- Can type 2 diabetes turn into type 1? No. Though they’re both forms of diabetes, they’re distinct and one cannot turn into the other.
- Can I lead a normal life with diabetes? Absolutely! With the right management, you can live a full and healthy life.
- What foods should diabetics avoid? Foods high in sugar, sodium, and unhealthy fats should be limited.
- Is diabetes genetic? Yes, genetics can play a role, especially in Type 1 diabetes. However, lifestyle factors are also crucial, particularly in Type 2 diabetes.
- Can diabetes be prevented? While you can’t prevent Type 1 diabetes, healthy lifestyle choices can help prevent Type 2 diabetes.
- What’s the difference between Type 1 and Type 2 diabetes? Type 1 is an autoimmune condition where the body attacks insulin-producing cells. Type 2, the more common type, occurs when your body becomes resistant to insulin or doesn’t produce enough.
- Can you get diabetes from eating too much sugar? Eating excessive sugar alone doesn’t cause diabetes. However, it can lead to obesity, a risk factor for Type 2 diabetes.
- Does diabetes have any symptoms? Yes, symptoms can include frequent urination, excessive thirst and hunger, fatigue, blurry vision, and slow-healing sores. However, some people with Type 2 diabetes may not exhibit symptoms.
- Can people with diabetes exercise? Absolutely! Regular physical activity is a vital part of diabetes management. It’s like a natural tune-up for your body, helping it use insulin more efficiently.
- Can diabetes cause mental health problems? Diabetes doesn’t directly cause mental health problems, but living with a chronic illness can increase the risk of conditions like depression and anxiety.
- What is gestational diabetes? It’s a type of diabetes that develops during pregnancy and usually goes away after the baby is born. However, it does increase the mother’s risk for Type 2 diabetes later in life.
- How often should I check my blood sugar levels? It depends on the type of diabetes and your treatment plan. Your healthcare provider will give you personalized advice.
- Can I drink alcohol if I have diabetes? In moderation and with your doctor’s approval, some people with diabetes can have alcohol. However, it’s important to understand it can affect blood sugar levels.
- What happens if I skip my diabetes medication? Skipping your medication can lead to high blood sugar levels, increasing your risk of diabetes complications. Always take medication as prescribed.
- Can diabetes be managed without medication? Some people with Type 2 diabetes can manage their condition with lifestyle changes alone, but many people need medication. Type 1 diabetes always requires insulin. Always follow your healthcare provider’s advice.
- Remember, each individual’s experience with diabetes can be different. It’s essential to have open and regular communication with your healthcare team to manage diabetes effectively.
My Concluding Thoughts on Diabetes Management
Like a journey, diabetes management isn’t a destination but a continuous process. It’s about steering the ship of your body through the waters of balanced diet, regular exercise, routine checkups, medication, and stress management. Yes, there might be storms (read: blood sugar spikes), but with the right tools and knowledge, you can sail through. So, take the helm, because your health is in your hands!


